Trends in Clinical and Medical Sciences
ISSN: 2791-0814 (online) 2791-0806 (Print)
DOI: 10.30538/psrp-tmcs2021.0011
Different treatment modalities in management of plantar fasciitis
Fluorent Lucotte, Ehab Ahmed\(^1\)
Department of Orthopaedics, Samarkand State University, Uzbekistan.; (F.L & E.A)
\(^{1}\)Corresponding Author: ehabahmed2k2@gmail.com
Abstract
Keywords:
1. Introduction
The plantar fascia is a broad band of fibrous tissue forming the medial longitudinal arch of the foot [1]. Plantar Fasciitis is an inflammatory condition which results in pain at the inferior aspect of the heel, affecting 10-15% of the general population [2]. Plantar fasciitis, a self-limiting condition, is a common cause of heel pain in adults [3]. It affects more than 1 million persons per year, and two-thirds of patients with plantar fasciitis will seek care from their family physician. Plantar fasciitis affects sedentary and athletic populations [4]. It is the most common cause of heel pain in the population aged above 40 years. Obesity, excessive foot pronation, excessive running, and prolonged standing are risk factors for developing plantar fasciitis [5].
It accounts for 10% of injuries in runners and is seen in both sedentary and athletic individuals. Patients with plantar fasciitis experience sharp or knife-like pain in the morning which subsides with a few initial steps [6]. However, the symptoms may also arise with prolonged standing which is sometimes accompanied by stiffness and in chronic case, the pain worsens by the end of the day limiting patient's daily activities [7].
Diagnosis is primarily based on history and physical examination. Patients may present with heel pain with their first steps in the morning or after prolonged sitting, and sharp pain with palpation of the medial plantar calcaneal region [8]. Discomfort in the proximal plantar fascia can be elicited by passive ankle/first toe dorsiflexion. Diagnostic imaging is rarely needed for the initial diagnosis of plantar fasciitis [9]. Use of ultrasonography and magnetic resonance imaging is reserved for recalcitrant cases or to rule out other heel pathology; findings of increased plantar fascia thickness and abnormal tissue signal the diagnosis of plantar fasciitis [10]. The use of oral non-steroidal anti-inflammatory drugs (NSAIDs) in reducing inflammation and providing pain relief has been tried. Silicone insole is a non-invasive modality that works by providing cushioning and add comfort to the sole as it absorbs 42% of shock while walking [11]. Considering this, we compared different treatment modalities in management of plantar fasciitis.
2. Methodology
Our study comprised of forty- five patients with plantar fasciitis (males- 25- females- 20). The study was approved from Ethical review committee. All patients within age limit 18-50 years were enrolled whereas patients with history of steroid injection, history of any surgery in the affected lower limb were not taken. Written consent was obtained.After recording demographic data of patients, randomization was performed based on computer. Group 1 patients received conventional treatment, group 2 patients received heat treatment with silicone heel pad and group 3 patients received active plantar fascia stretching with sham calf stretching. Patient was evaluated using foot function index (FFI) and the foot and ankle disability index (FADI) to know the baseline scores of pain, disability and restrictions in activities of daily living. 3 sub-scales such as pain, disability, and activity restriction, each item evaluated on a scale of 0-10. Results of the present study after recording all relevant data were subjected for statistical inferences using One-way ANOVA test. The level of significance was significant if p value was below 0.05.
3. Results
One-way ANOVA test
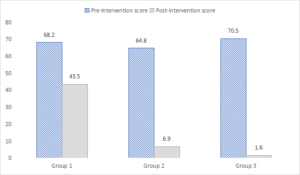
In group 1, foot function pre-intervention index score and post-intervention score was 68.2 and 43.5, in group 2 was 64.8 and 6.9 and in group 3 was 70.5 and 1.6 respectively. A significant difference was observed (P< 0.05) (Table 1, Figure 1).
Table 1. Comparison of foot function index score.
| Groups | Pre-intervention score | Post-intervention score | P value |
|---|---|---|---|
| Group 1 | 68.2 | 43.5 | < 0.05 |
| Group 2 | 64.8 | 6.9 | < 0.05 |
| Group 3 | 70.5 | 1.6 | < 0.05 |
Figure 1. Graphical comparison of foot function index score
One-way ANOVA test
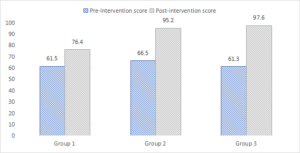
In group 1, pre-intervention foot and ankle disability score and post-intervention score was 61.5 and 76.4, in group 2 was 66.5 and 95.2 and in group 3 was 61.3 and 97.6 respectively. A significant difference was observed (P< 0.05) (Table 2, Figure 2).
Table 2. Foot and ankle disability index.
| Groups | Pre-intervention score | Post-intervention score | P value |
|---|---|---|---|
| Group 1 | 61.5 | 76.4 | < 0.05 |
| Group 2 | 66.5 | 95.2 | <0.05 |
| Group 3 | 61.3 | 97.6 | < 0.05 |
Figure 2. Graphical comparison of foot and ankle disability index
4. Discussion
We compared different treatment modalities in management of plantar fasciitis. We created 3 groups of 15 each. Group 1 patients received conventional treatment, group 2 patients received heat treatment with silicone heel pad and group 3 patients received active plantar fascia stretching with sham calf stretching.Plantar fasciitis is a common cause of heel pain in adults [12]. It is estimated that more than 1 million patients seek treatment annually for this condition, with two-thirds going to their family physician [13]. Plantar fasciitis is thought to be caused by biomechanical overuse from prolonged standing or running, thus creating microtears at the calcaneal enthesis [14]. Some experts have deemed this condition "plantar fasciosis," implying that its etiology is a more chronic degenerative process versus acute inflammation [15].
Our results demonstrated that in group 1, foot function pre-intervention index score and post-intervention score was 68.2 and 43.5, in group 2 was 64.8 and 6.9 and in group 3 was 70.5 and 1.6 respectively. Gupta et al., [16] in their study on 140 patients of plantar fasciitis were divided into four groups with 35 patients each. Patients in four groups received analgesics, hot water fomentation and silicon heel pads, plantar fascia stretching and calf stretching exercises, respectively. Heel pain was evaluated using foot function index (FFI) and disability using foot and ankle disability index (FADI). Clinical evaluation was done weekly up to a period of 4 months and then at 6 months, 8 months, 10 months and 12 months. Mean age of patients was \(43.4 \pm 10.6\) years with average duration of symptoms being 27.26 weeks (range 4-200 weeks). Both FFI and FADI showed statistically significant improvement at 12 months in all the four groups (p value < 0.0001 for all groups). However, groups 2, 3 and 4 were observed to show statistically better results in terms of heel pain reduction (FFI) as compared to group 1 (ANOVA, p value < 0.0001 for group 1 vs. 2, group 1 vs. 3 and group 1 vs. 4). In terms of disability (FADI), best results were observed in group 3.
Our results showed that in group 1, pre-intervention foot and ankle disability score and post-intervention score was 61.5 and 76.4, in group 2 was 66.5 and 95.2 and in group 3 was 61.3 and 97.6 respectively. In a randomized controlled trial by Pfeffer et al., [17] on 236 patients, the comparison was made between three prefabricated shoe inserts (a rubber heel cup, a felt insert and a silicone heel pad) along with Achilles tendon and plantar fascia stretching and stretching alone. Only 190 patients completed the 8 weeks follow-up, the response rates were found to be better in the silicone insert group than in the stretching-only group \((p=0.019)\). Although, the silicone insert group was shown to improve more on FFI as compared to stretching alone, but there was no significant difference \((p=0.54)\).
Donley et al., [18] in their study twenty-nine patients with the diagnosis of plantar fasciitis were treated with a conservative regimen that included heel-cord stretching, viscoelastic heel cups, and night splinting. They were randomly assigned to either a placebo group or an NSAID group. In the NSAID group, celecoxib was added to the treatment regimen. Pain and disability mean scores improved significantly over time in both groups, although there was no statistical significance between the placebo and NSAID groups at 1, 2, or 6 months. There was a trend towards improved pain relief and disability in the NSAID group, especially in the interval between the 2 and 6-month follow up. Pain improved from baseline to 6 months by a factor of 5.2 and disability by 3.8 in the NSAID group compared to 3.6 and 3.5, respectively, in the placebo group. Even though at baseline the pain and disability scores were higher in the NSAID group, the final pain and disability scores were subjectively lower in the NSAID group than in the placebo group (1.43 for pain and 1.16 for disability in the NSAID group, compared to 1.86 and 1.49, respectively, in the placebo group).
Radford et al., [19] in their study ninety-two participants with plantar heel pain were recruited and were randomly allocated to an intervention group that were prescribed calf muscle stretches and sham ultrasound (n = 46) or a control group who received sham ultrasound alone (n = 46). Primary outcome measures were 'first-step' pain (measured on a 100 mm Visual Analogue Scale) and the Foot Health Status Questionnaire domains of foot pain, foot function and general foot health. Both treatment groups improved over the two weeks period of follow-up but there were no statistically significant differences in improvement between groups for any of the measured outcomes. For example, the mean improvement for 'first-step' pain (0-100 mm) was -19.8 mm in the stretching group and -13.2 mm in the control group. For foot function (0-100 scale), the stretching group improved 16.2 points and the control group improved 8.3 points. Ten participants in the stretching group experienced an adverse event, however most events were mild to moderate and short-lived.
5. Conclusion
Results of our study showed that active plantar fascia stretching with sham calf stretching exercise resulted in most significant improvement in FFI and FADI score followed by treatment with heat and silicone heel pad and conventional treatment.Author Contributions
All authors contributed equally to the writing of this paper. All authors read and approved the final manuscript.Conflicts of Interest
"The authors declare no conflict of interest.''References
- Sharma, N., & Singh, G. (2010). Splinting and stretching for plantar fasciitis pain. Lower Extremity Review, 10, 15-19. [Google Scholor]
- Furey, J. G. (1975). Plantar fasciitis. The painful heel syndrome. The Journal of bone and joint surgery. American Volume, 57(5), 672-673. [Google Scholor]
- Lapidus PW, Guidotti FP. Painful heel: Report of 323 patients with 364 painful heels. Clinical Orthopaedics and Related Research. 1965;39:178-186. [Google Scholor]
- Digiovanni, B. F., Nawoczenski, D. A., Malay, D. P., Graci, P. A., Williams, T. T., Wilding, G. E., & Baumhauer, J. F. (2006). Plantar fascia-specific stretching exercise improves outcomes in patients with chronic plantar fasciitis: a prospective clinical trial with two-year follow-up. JBJS, 88(8), 1775-1781. [Google Scholor]
- Donley, B. G., Moore, T., Sferra, J., Gozdanovic, J., & Smith, R. (2007). The efficacy of oral nonsteroidal anti-inflammatory medication (NSAID) in the treatment of plantar fasciitis: a randomized, prospective, placebo-controlled study. Foot & Ankle International, 28(1), 20-23. [Google Scholor]
- Martin, J. E., Hosch, J. C., Goforth, W. P., Murff, R. T., Lynch, D. M., & Odom, R. D. (2001). Mechanical treatment of plantar fasciitis: a prospective study. Journal of the American Podiatric Medical Association, 91(2), 55-62. [Google Scholor]
- Young, C. C., Rutherford, D. S., & Niedfeldt, M. W. (2001). Treatment of plantar fasciitis. American Family Physician, 63(3), 467-474. [Google Scholor]
- Carlson, R. E., Fleming, L. L., & Hutton, W. C. (2000). The biomechanical relationship between the tendoachilles, plantar fascia and metatarsophalangeal joint dorsiflexion angle. Foot & Ankle International, 21(1), 18-25. [Google Scholor]
- Crawford, F., & Thomson, C. E. (2003). Interventions for treating plantar heel pain. Cochrane Database of Systematic Reviews, (3). https://doi.org/10.1002/14651858.CD000416. [Google Scholor]
- Rompe, J. D., Cacchio, A., Weil Jr, L., Furia, J. P., Haist, J., Reiners, V., ... & Maffulli, N. (2010). Plantar fascia-specific stretching versus radial shock-wave therapy as initial treatment of plantar fasciopathy. JBJS, 92(15), 2514-2522. [Google Scholor]
- Petrofsky, J. S., Laymon, M. S., Alshammari, F., & Khowailed, I. A. (2014). Evidence based use of heat, cold and NSAIDS for plantar fasciitis. Clinical Research on Foot & Ankle, 2, Article No. 140. https://doi.org/10.4172/2329-910X.1000140.[Google Scholor]
- Gill, L. H., & Kiebzak, G. M. (1996). Outcome of nonsurgical treatment for plantar fasciitis. Foot & Ankle International, 17(9), 527-532. [Google Scholor]
- Biswas, C., Pal, A., & Acharya, A. (2011). A comparative study of efficacy of oral nonsteroidal antiinflammatory agents and locally injectable steroid for the treatment of plantar fasciitis. Anesthesia, Essays and Researches, 5(2), 158-161. [Google Scholor]
- Tisdel, C. L., Donley, B. G., & Sferra, J. J. (1999). Diagnosing and treating plantar fasciitis: a conservative approach to plantar heel pain. Cleveland Clinic Journal of Medicine, 66(4), 231-235. [Google Scholor]
- Singh, D., Angel, J., Bentley, G., & Trevino, S. G. (1997). Fortnightly review: Plantar fasciitis. BMJ, 315(7101), 172-175. [Google Scholor]
- Gupta, R., Malhotra, A., Masih, G. D., Khanna, T., Kaur, H., Gupta, P., & Kashyap, S. (2020). Comparing the role of different treatment modalities for plantar fasciitis: a double blind randomized controlled trial. Indian journal of Orthopaedics, 54(1), 31-37. [Google Scholor]
- Pfeffer, G., Bacchetti, P., Deland, J., Lewis, A. I., Anderson, R., Davis, W., ... & Smith, R. (1999). Comparison of custom and prefabricated orthoses in the initial treatment of proximal plantar fasciitis. Foot & Ankle International, 20(4), 214-221. [Google Scholor]
- Donley, B. G., Moore, T., Sferra, J., Gozdanovic, J., & Smith, R. (2007). The efficacy of oral nonsteroidal anti-inflammatory medication (NSAID) in the treatment of plantar fasciitis: a randomized, prospective, placebo-controlled study. Foot & Ankle International, 28(1), 20-23. [Google Scholor]
- Radford, J. A., Landorf, K. B., Buchbinder, R., & Cook, C. (2007). Effectiveness of calf muscle stretching for the short-term treatment of plantar heel pain: a randomised trial. BMC Musculoskeletal Disorders, 8(1), 1-8. [Google Scholor]